Machine Learning and More: PC3I at ASCO
May 28, 2020
Most patients with cancer die without ever having a high-quality conversation with their doctor about their values, goals, and care preferences—what is called a "serious-illness conversation".
Research shows that increasing serious-illness conversations between clinicians and patients makes it more likely that patients will receive care consistent with their preferences in their last year of life. Penn Center for Cancer Care Innovation (PC3I) Fellow Chris Manz, MD, Faculty member Ravi Parikh, MD, Director Justin Bekelman, MD, and co-authors across Penn created and studied an intervention to deliver machine learning-based mortality estimates with behavioral nudges to oncologists. The intervention significantly increased serious illness conversations between doctors and their patients by three-fold over 16 weeks. On Friday, their presentation of these findings will be available on-demand to ASCO20 Virtual attendees.
Every year, the Annual Meeting of the American Society of Clinical Oncology (ASCO) brings together oncology professionals from around the world to deliver the latest cancer science. The 2020 program will feature the following presentations co-authored by PC3I Faculty and Fellows:
1. Machine learning and behavioral nudges increase serious illness conversations
- Title: Effect of integrating machine learning mortality estimates with behavioral nudges to increase serious illness conversions among patients with cancer: A stepped-wedge cluster randomized trial.
- PC3I authors: Chris Manz, MD, Justin E. Bekelman, Ravi B. Parikh
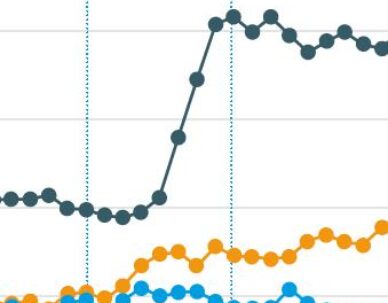
- Conclusions: An intervention consisting of machine learning mortality estimates and behavioral nudges to oncology clinicians increased serious-illness conversations by three-fold over 16 weeks, a significant difference. This is one of the first studies evaluating a machine learning-based behavioral intervention to improve serious illness communication in oncology. Secondary analyses (completed April 2020) will clarify whether this intervention leads to a sustained increase in SIC rates and improves goal-concordant care and end-of-life outcomes.
2. Patient-reported outcome collection as standard-of-care
- Title: Implementing routine patient-reported outcome collection in a large, academic health system.
- PC3I authors: Peter E. Gabriel
- Conclusions: Routine patient-reported outcome collection as standard-of-care is possible across a variety of practice environments in a large, complex health system, with sustained capture of approximately three-fourths of eligible visits. Most patients prefer to complete the questionnaire in clinic.
3. Machine learning model predicts short-term mortality
- Title: Prospective validation of a machine learning algorithm to predict short-term mortality among outpatients with cancer.
- PC3I authors: Chris Manz, Justin E. Bekelman, Ravi B. Parikh
- Conclusions: In this prospective cohort study among outpatients with cancer, a machine learning (ML) prognostic algorithm based on EHR data had better discrimination and calibration than published cancer-specific models. This is one of the first ML prognostic models to be prospectively validated in oncology.
4. Improved cardiovascular disease risk mitigation needed for androgen deprivation therapy recipients
- Title: Assessment and management of cardiovascular risk factors among U.S. Veterans with newly diagnosed prostate cancer.
- PC3I authors: Ravi B. Parikh, Samuel U. Takvorian
- Conclusions: Cardiovascular disease (CVD) risk factor assessment in Veterans with prostate cancer has increased over time. However, androgen deprivation therapy (ADT) does not appear to meaningfully impact CVD assessment or management, despite its known association with CVD risk. Over half of patients initiating ADT had elevated CVD risk factor(s). Multi-disciplinary efforts to improve CVD risk mitigation are needed among men initiating ADT.
5. Utilization management policy and increased evidence-based, patient-friendly radiation
- Title: Impact of utilization management policy on uptake of hypofractionated radiation in early-stage breast cancer.
- PC3I authors: Ravi B. Parikh, Justin E. Bekelman
- Conclusions: A payer’s utilization management policy was associated with direct and spillover increases in HFR use, even after accounting for a strong secular trend towards increased hypofractionation use. However, policymakers must balance the impact of this and similar policies against their additional administrative costs.
6. NCI and academic hospitals have less timely cancer treatment
- Title: Association of hospital type and patient volume growth with timely cancer treatment.
- PC3I authors: Zachary A.K. Frosch, Justin E. Bekelman, Samuel U Takvorian
- Conclusions: Patients with newly diagnosed cancer are increasingly receiving treatment at the National Cancer Institute (NCI) and academic hospitals. While time to treatment initiation at NCI and academic hospitals is longer than in the community, patient volume growth has been possible without delaying cancer treatment. Further study is needed to determine whether continued growth at this rate is sustainable. *Received merit award
7. Pay-for-performance program and increased evidence-based prescribing
- Title: Association between a national insurer’s pay-for-performance program for oncology and changes in prescribing of evidence-based cancer drugs and spending.
- PC3I authors: Justin E. Bekelman
- Conclusions: A national insurer’s oncology pay-for-performance program was associated with a 5.1 percentage point increase in prescribing of evidence-based cancer drug regimens. Our findings suggest that pay-for-performance programs may be effective in increasing evidence-based cancer drug prescribing at national scale — enhancing cancer care quality. However, they may also increase out-of-pocket expenses and may not lead to savings in total health care spending during the 6-month episode.
8. Immune checkpoint inhibitors and increased systemic therapy at end of life
- Title: The adoption of immune checkpoint inhibitors and patterns of care at the end of life.
- PC3I authors: Ravi B. Parikh, Ronac Mamtani
- Conclusions: The adoption of immune checkpoint inhibitors was associated with a substantive increase in the use of systemic therapy at end of life in melanoma, and a smaller yet significant increase in non-small cell lung cancer.