Payer Policy Increases Use of Evidence-Based Radiation
May 6, 2020

Research by PC3I Innovation faculty, affiliates, and their partners into the effect of payer policies on the use of evidence-based breast cancer treatment recently featured in articles by The ASCO Post and Physician’s Weekly. Led by Ravi Parikh, MD, the study found that a large utilization management payer program improved the use of short-course, patient-friendly, evidence-based radiation in breast cancer among women both directly and indirectly subject to the policy.
In the United States, breast cancer ranks highest among cancers in terms of costs. In 2011, the American Society for Radiation Oncology (ASTRO) recommended hypofractionated radiotherapy for women older than 50 years with early-stage breast cancer. In 2018, it expanded its recommendation to nearly all patients with localized breast cancer. Hypofractionated radiotherapy after breast-conserving surgery is a cost-effective, convenient, and evidence-based treatment strategy for patients with early-stage breast cancer. Three years after the initial recommendation, however, less than 40% of women who were eligible for the therapy were receiving it.

In the study published by JAMA Oncology, Parikh and colleagues conducted a retrospective economic analysis of claims data from January 2012 to June 2018 for women with early-stage breast cancer who were eligible for hypofractionated radiotherapy. Beginning on January 1, 2016, the payer instituted a utilization management policy to encourage use of hypofractionated, or short-course, radiation among women in fully insured plans. Under the policy, claims for extended-course radiotherapy were not reimbursed for fully insured women who were eligible for hypofractionated radiotherapy. The policy did not apply to women in self-insured plans. “Utilization management is sometimes a dirty word in healthcare and especially cancer care,” says Parikh. “But we suggest there are times that it can be used to promote evidence-based practice–and have powerful and positive spillover effects.”
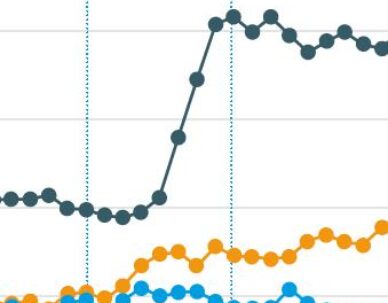
A total of 10,540 eligible women were identified. 3,619 (34.3%) were in fully insured plans and therefore subject to the utilization management policy. Taking into consideration the general trend toward improved uptake in hypofractionated radiotherapy, adjusted difference-in-differences analysis showed the policy was associated with a significant increase of 4.2% (P=.05) in this therapy among fully insured patients and a nonsignificant decrease of $2,275 in radiotherapy-related spending (P=.09). Spillover analyses of self-insured patients, who were indirectly exposed to the policy through clinicians who also treated fully insured patients, revealed a significantly higher uptake of the short-course radiotherapy (8.5%; P<.001) compared with those who were not exposed.
This study suggests that a payer’s utilization management policy was associated with direct and spillover increases in the use of hypofractionated radiotherapy, even after accounting for a long-term secular trend in the uptake of hypofractionated radiotherapy in the control groups.
Ravi Parikh, MD and colleagues
“Utilization management may promote evidence-based cancer care,” they concluded.
This article references the following publication:
Association of utilization management policy with uptake of hypofractionated radiotherapy among patients with early-stage breast cancer. DOI: 10.1001/jamaoncol.2020.0449.