Nudging in Cancer Care: A Panel Discussion of PC3I Experts
November 6, 2019
The Symposium panel was one of two days of events for health system executives and health services research scientists interested in the latest developments in the rapidly expanding use of behavioral insights or “nudges” to influence the behavior of clinicians or their patients in cancer and other fields of medical care.
A survey of last year’s Nudges in Health Care Symposium attendees found that they were keenly interested in hearing from clinician researchers who were directly involved in designing, testing and using nudges. A response to that request, this year’s panel included Christopher Manz, MD, a Fellow in Penn Medicine’s Hematology/Oncology Department; Rinad Beidas, PhD, Director of the Penn Implementation Science Center; Justin Bekelman, MD, Director of the Penn Center for Cancer Care Innovation; and M. Kit Delgado, MD, MS, Director of the Penn Behavioral Science and Analytics for Injury Reduction (BeSAFIR) Lab. The four are either innovation faculty, innovation fellows or members of the PC3I advisory group.
Manz is part of a research team focused on developing better ways of estimating when cancer patients are likely to die. There is currently no consistently accurate way to do this even though having that estimate could nudge physicians to schedule serious illness conversations.
“One of the challenges we face in oncology is trying to ensure that the care we deliver to patients near the end of life is consistent with their goals and wishes,” Manz told the symposium audience. “That seems like a fairly obvious and simple thing to deliver, but nationwide, greater than 90% of cancer patients actually die without any documented conversation about the type of care or their end-of-life preferences would be.
“There are a number of reasons why having a documented conversation about end of life preferences is a good thing for patients,” Manz continued. “Patients who have these conversations with their providers are less likely to die in a hospital or in an ICU. They’re less likely to get chemo at the end of life. They’re more likely to get hospice services. And having these conversations actually improves anxiety and depression scores.”
Manz said one of the reasons these conversations so often fail to happen is that doctors don’t have a dependable way to predict which of their patients are at the highest risk of dying in the next six months.
He is part of a team that created a big data and algorithm system to identify cancer patients who are at high risk, and then systematically use electronic health record, email or text messaging to nudge their physicians toward scheduling an end-of-life conversations.
“The initial results have been promising and in some of our pilots, we’ve seen an increase in the number of documented discussions about end-of-life care preferences to an extent that it’s been sustained after the intervention as well,” Manz said.
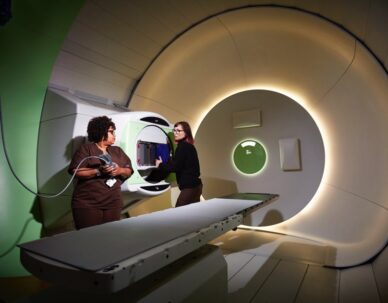
Panelist Justin Bekelman, a radiation oncologist who heads PC3I, spoke of nudges in cancer care from the 30,000 foot view and cited five lessons researchers have learned so far.
- The goal is to solve problems that matter. Nudges actually solve problems.
- When thinking through and designing a potential clinical nudge, it’s crucial to collect as much information and insights from providers and patients as possible. Understand the problem from their lived experience and what actually needs to be nudged. It’s common for scientists to work on assumptions and nudge the wrong thing.
- When designing nudges, turn up the dial as high as you can without making patients or clinicians mad at you.
- When thinking about implementing a dialed up nudge, be sure you really understand the target clinicians’ workflow. If there’s a second click in the EHR or something else the provider has to click to get into the nudge, it going to be less effective.
- If you can’t quite bake a nudge into the workflow, don’t give up. Don’t abandon the project. Think of something that approaches the nudge effect and don’t let the perfect be the enemy of the good. You may at least learn something that will enable you to ultimately work and scale the nudge into the workflow in the future.